Patients win when they have the choice to receive medical care from an expert physician. Increasingly however, health systems, hospitals, and clinics are replacing or supplanting highly-trained physicians with nurse practitioners (NPs) and other non-physician providers. Nurse practitioners have only a small fraction of the formal education and training that physicians receive in medical school and residency, yet are allowed to evaluate patients, order tests, and prescribe medications, often with minimal or no physician oversight depending on state laws. Patients shouldn’t have to settle for anything less than the very best when their life is hanging in the balance.
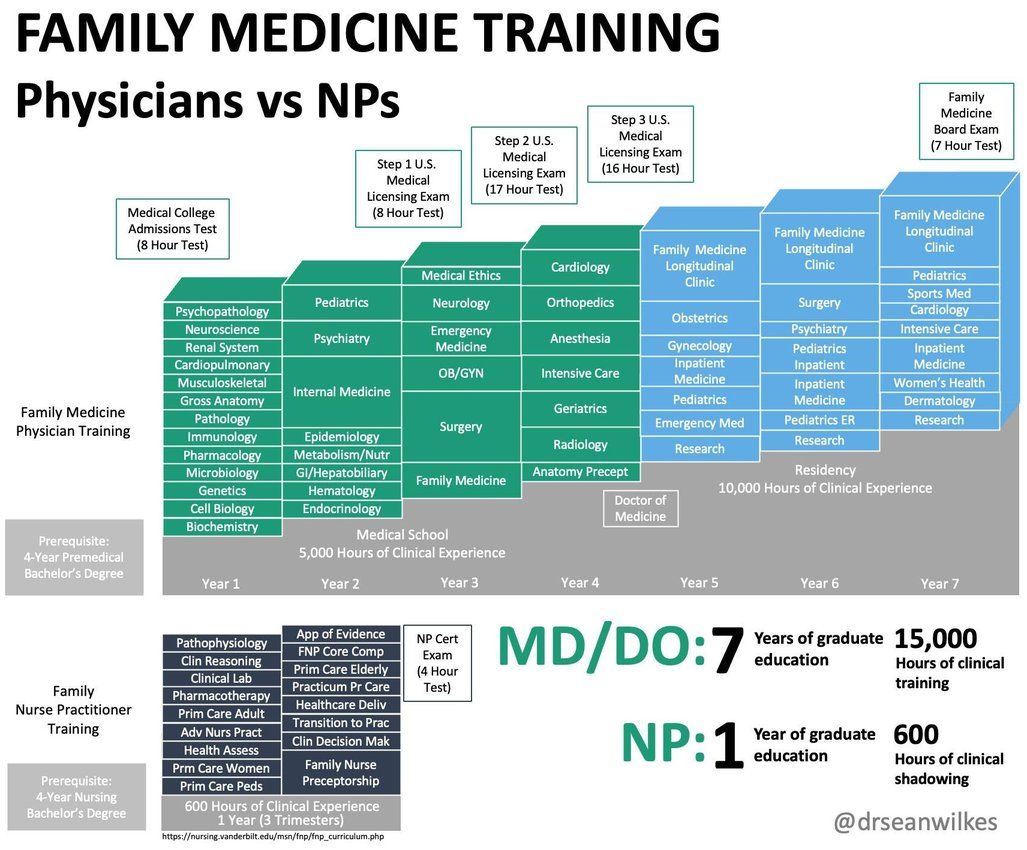
Nurse practitioners have a mere fraction of the knowledge, training, and experience of physicians, who spend upwards of 15,000 hours in medical school, residency, and fellowship and must pass rigorous board and specialty certification exams. By contrast, NPs obtain their degrees through loosely structured and highly variable programs - programs that are often 100% online and offered by diploma mills that accept virtually all applicants - and may graduate with as little as 500 hours of clinical exposure. This is less hands-on time than what PetSmart dog groomers and barbers in many states are required to have. Does this sound like the type of healthcare provider you would entrust your life to?

Stories abound of nurse practitioners missing life-threatening diagnoses, resulting in patient harm or death. From the failure to recognize pneumonia and sepsis in the tragic case of 7-year-old Betty Wattenbarger, to the needless death of 19-year-old Alexis Ochoa-Dockins due to a missed diagnosis of pulmonary embolism, it is clear that nurse practitioners lack the necessary foundation in medical education to develop the clinical acumen honed by physicians after years and years of training. There are no shortcuts in medicine, and diseases do not magically simplify themselves and become easier to diagnose and treat in the absence of a physician. Yet, more than 20 states and the District of Columbia grant nurse practitioners Full Practice Authority - the legal right to evaluate and diagnose patients, order and interpret tests, and prescribe medications and controlled substances. Think that sounds suspiciously like the practice of medicine? Unfortunately, nurse practitioners are licensed under the boards of nursing, and the state medical boards are powerless in cases of nurse practitioner malpractice or misconduct.

From playing make-believe and masquerading as doctors, to consulting social media and soliciting medical advice on Facebook when they don’t know what to do, to instances of outright illegal behavior, examples of nurse practitioners engaging in unprofessional conduct are abundant. And even when they are behaving, there’s no evidence that they are capable of providing high-quality, cost-efficient care on par with physicians, especially when practicing independently. No head-to-head, randomized controlled trials have been conducted comparing NPs versus physicians. However, data exists showing that NPs prescribe more antibiotics, place lower-quality specialist referrals, and order more diagnostic imaging when compared to physicians. Yet under the majority of insurance plans and healthcare billing schemes in the United States, patients pay the same amount whether they see a nurse practitioner or a physician. Why pay the same for a lower-quality product?
Don’t settle for someone who “practices healthcare”.
It’s OK to ask for a physician.

*not affiliated with or endorsed by the authors

*not affiliated with or endorsed by the authors